
The Ketogenic Diet: Does it live up to the hype?

If you believe the buzz, ketosis—whether via the almost-zero-carb ketogenic diet or via ketone supplements—can curb appetite, enhance performance, and cure nearly any health problem that ails you. Sound too good to be true? It probably is.
Maybe with a side of guacamole and some shredded cheese on top?
“I’m doing this for my health,” you could purr virtuously, as you topped your delectably marbled, medium-rare steak with a fried egg.
Well, many advocates of the ketogenic diet argue exactly that: By eating a lot of fat and close to zero carbohydrates you too can enjoy enhanced health, quality of life, performance, brain function, and abs you can grate that cheese on.
So, in this article, we’ll explore:
- What are ketones, and what is ketosis?
- What, exactly, is a ketogenic diet?
- What evidence and scientific research supports the ketogenic diet?
- Do ketone supplements work?
- Is the ketogenic diet or ketone supplementation right for me?
How to read this article
If you’re just curious about ketogenic diets:
- Feel free to skim and learn whatever you like.
If you want to change your body and/or health:
- You don’t need to know every detail. Just get the general idea.
- Check out our advice at the end.
If you’re an athlete interested in performance:
- Pay special attention to the section on athletic performance.
- Check out our advice for athletes at the end.
If you’re a fitness pro, or interested in geeking out with nutritional science:
- We’ve given you some “extra credit” material in sidebars throughout.
- Check out our advice for fitness pros at the end.
It all started with the brain.
If you’ve called Client Care at Precision Nutrition, you might have spoken to Lindsay.
Aside from being an incredibly helpful and friendly voice on the other end of the phone, Lindsay is also a tireless advocate for a health condition that has shaped her life in many ways: epilepsy.
Epilepsy is an ancient brain phenomenon, known to medicine thousands of years ago. To manage it, our Neolithic ancestors drilled holes in one another’s skulls, perhaps trying to let the bad stuff out—a practice known as trepanation.
Around 400 BCE, the ancient Greek doctor Hippocrates observed a man who had seizures for five days. On the sixth day, he noted, as the patient “abstained from everything, both gruel and drink, there were no further seizures.”
About 1,400 years later, in 1000 CE, the famous Persian physician Avicenna—who coined the term “epilepsy”, from the ancient Greek verb epilambanein (to seize or attack, as the neurological condition caused seizures), speculated that “overfeeding” might be a risk factor for epilepsy.
By 1911, a pair of Parisian doctors were trying fasting as a treatment for children with epilepsy, and in the United States, physical culturist Bernarr McFadden was claiming that fasting for three days to three weeks could cure anything.
Despite not having the tools and insight of modern neuroscience, these and other people who explored fasting and dietary prescriptions for neurological disorders were on to something.
We now know that there may be a dietary connection—not just between epilepsy and what we eat (or don’t), but also with many other brain disorders.
Unfortunately, fasting isn’t fun. We evolved with a pretty strong aversion to starvation, and our brains and GI tracts have lots of ways to make sure we eat enough.
Which raises the question:
Could we get the health benefits of fasting another way?
In other words:
Could there be “fasting without fasting”?
In 1921, two things happened.
One: Endocrinology researcher Rollin Woodyatt noted that the same chemical environment happened with both starvation and a diet that was very low in carbohydrates and very high in fat.
Two: Dr. Russell Wilder wondered:
Could a person get the health benefits of fasting without actually fasting?
He and other doctors at the Mayo Clinic experimented with what Wilder called the “ketogenic diet” during the early 1920s. Not only did children with epilepsy seem to improve overall with this type of diet, they seemed to think and behave better as well.
Proven by several notable medical authorities, a ketogenic diet as a treatment for childhood epilepsy found its way into medical textbooks by around 1940, and stayed there throughout the 20th century.
Nowadays, aging, contact sports, and modern warfare present us with new populations of people whose brains might benefit from a ketogenic diet:
- people with neurodegenerative disorders (such as multiple sclerosis, Parkinson’s, and Alzheimer’s); and
- people with traumatic brain injury (TBI) from events such as explosions or concussions.
First the brain, then the body.
There was another group of people who became curious about ketogenic diets some time in the 1980s and 1990s: bodybuilders and physique athletes.
These folks weren’t too concerned about brain health or longevity. They wanted to be ripped.
The ketogenic diet seemed like a magic bullet: a way to eat butter, bacon and cream, and still get abs.
Today, what’s old is new again.
Physique- and performance-conscious people, as well as people looking to maximize lifespan and life quality, have rediscovered this old-school dietary paradigm and are wondering:
- Could a ketogenic diet help me perform better?
- Could a ketogenic diet help me live longer?
- Could a ketogenic diet help me look great on the beach?
The answer?
It depends. (Don’t you hate that? But it’s true.)
To understand why, we’ll look at:
- the science of ketosis;
- what a ketogenic diet looks like in “real life”;
- who it might work for (and might not work for); and
- what this means for you.
Let’s start by clarifying just what a ketogenic diet is.
What does a ketogenic diet look like?
It might be hard to translate “low carb, high fat” into everyday foods.
To give you a better idea of the ketogenic diet in real life, here’s a comparison:
| Protein | Carb | Fat | |
|---|---|---|---|
| PN Mixed Meal | ~30% | ~40% | ~30% |
| Paleo Meal | ~40% | ~20% | ~40% |
| Low-Carb Meal | ~40% | ~10% | ~50% |
| Ketogenic Meal | ~20% | ~5% | ~75% |
And here’s what that might look like translated into meals.
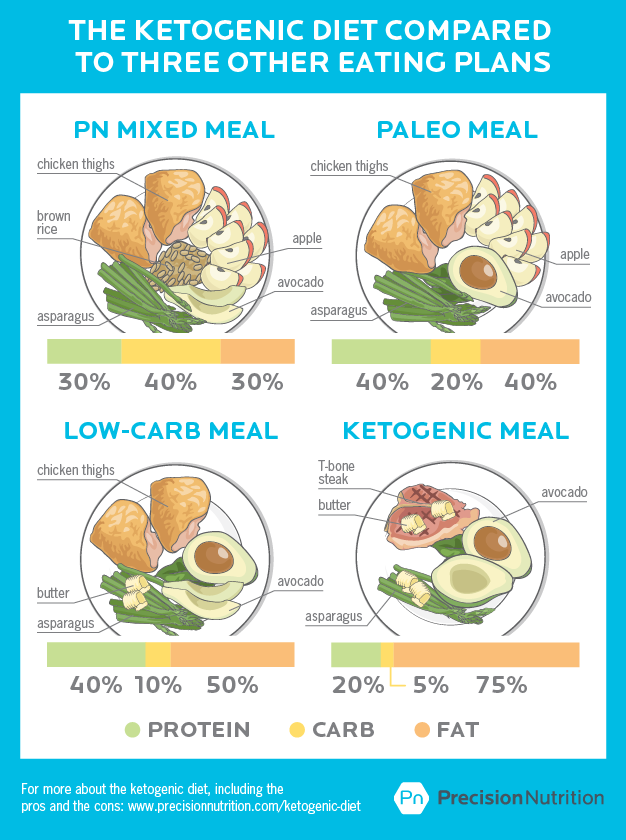
Notice a few things.
Protein
For the first three meals, protein is more or less the same, with a little variation.
Ketogenic diets, on the other hand, include less protein—usually closer to 10 or 20 percent of total daily intake.
Extremely low in carbohydrates
The Precision Nutrition plate suggests high-fiber, slow-digesting carbohydrates, such as whole grains, beans and legumes, fruits, and starchy vegetables.
The Paleo plate may contain slightly fewer carbohydrates (early human diets often had plenty of them), but eliminates the grains and beans / legumes.
The “low carb” plate will have fewer carbohydrates than the first two, but still have a small amount, likely from vegetables.
The ketogenic meal shoots for near-zero carbs. Most estimates suggest around 10-15 grams of carbs a day. To give you an idea of what this looks like, that’s about one fist-sized portion of cooked carrots, or about 10-15 grapes. For the whole day.
Very high in fat
The Precision Nutrition plate suggests about 1-2 thumb-sized portions of fat-dense foods (like nuts, cheese, avocado, olive oil, etc.) per meal, depending on body size, activity level, and goals.
The Paleo and low-carb plates may be roughly similar, with a little variation.
We might call all three of these “moderate fat”. Indeed, some indigenous diets (aka variations on the “Paleo” concept) are often quite low in fat, especially saturated fat.
The ketogenic meal, on the other hand, is high fat—even up to 90 percent of total energy intake. That means if you’re eating a 500-calorie spinach and mushroom salad, you get about 2 thumb-sized pieces of chicken breast on top, and then pour about 3-4 glugs of olive oil on top… Yum yum!
Highly restrictive
A ketogenic diet is the most restrictive and limited of all four of these styles of eating. Here’s what you can eat on a ketogenic diet:
A small amount of protein, such as:
- meat
- poultry
- fish
- seafood
- eggs
A large amount of high-fat foods, such as:
- avocado
- coconut and coconut milk or oil
- olive oil and any other oil
- nuts and nut butters
- bacon
- egg yolks
- butter
- cheese
A very small amount of very-low-carbohydrate vegetables, such as:
- leafy greens
- brassicas: broccoli, cauliflower, Brussels sprouts, cabbage
- asparagus
- cucumber
- celery
- tomatoes
- peppers
- mushrooms
- zucchini
Here’s what you can’t eat on a ketogenic diet:
- Most dairy (except high-fat items like butter and certain cheeses)
- Fruit
- Grains
- Beans and legumes
- Starchy vegetables (such as sweet potatoes)
- Slightly-sweet vegetables such as winter squash, beets, or carrots
- Most processed foods (with the notable exception of pork rinds)
So, let’s recap:
Ketogenic menus:
- Vary in the proportion of protein but are generally low.
- Stay as close to no-carb as possible.
- Are very high in fat.
- Are very limited in food choices.
So why go to all this effort?
Well, for particular groups of people, ketosis may indeed be helpful.
(For other people, of course, it may not be helpful… and it may be actively harmful. We’ll talk more about that in a moment.)
To understand why this is true, let’s look at how ketosis actually works.
What is ketosis?
The role of ketones
Ketones are a group of organic compounds with a specific structure.
The term “ketone” was actually coined around 1850 by German chemist Leopold Gmelin, along with the term “ester”. (See? Not as new as you’d think!)
We can use two types of ketones as energy sources, acetoacetate and D-β-hydroxybutyrate. (The β sign means “beta”.)
Our body can make ketones through a complex biochemical pathway.
The pathway to ketosis
Put very simply, when the conditions are right (for instance, during starvation or fasting, or when our carb intake is very low):
- Our body releases fatty acids from our stored body fat.
- These fatty acids enter other cells.
- Fatty acids are combined with co-enzyme A to form acetyl-CoA chains.
- These chains move into the mitochondria (our cells’ energy factories).
- The chains are broken down into acetyl-CoA units by a sequence of reactions known as β-oxidation.
- Chemical magic happens.
- Acetyl-CoA forms your friends the ketones: acetoacetate and β-hydroxybutyrate, along with acetone (the same smelly stuff in your nail polish remover).
- Ketones are released by the liver into the blood.
- Almost any cell that needs energy can grab it from these circulating ketones. Again, our brain will be the greediest for these nummy little molecules.
The shape and orientation of molecules is important.
Stereoisomers are molecules with the same chemical makeup, but different shapes and configurations. You can imagine your right hand as a “stereoisomer” of your left: they both share the same components, just arranged differently.
Shape and orientation matter to molecules and their actions, just like having right-handed and left-handed gloves or shoes matters.
The ketone D-β-hydroxybutyrate is not the same as its stereoisomer L-β-hydroxybutyrate.
This difference in molecular configuration matters for several parts of the conversion process.
For instance, when D-β-hydroxybutyrate is converted back to acetyl-CoA, its intermediate form D-β-hydroxybutyrate-CoA isn’t the same thing as L-β-hydroxybutyrate-CoA (an intermediate of β- oxidation).
Each stereoisomer uses different enzymes for conversion, much like each lock has its own unique key.
This difference also matters for ketone supplementation (see below).
You want to supplement the right stereoisomer, rather than a random pile of ketone types. Usually in test tube chemistry, you get a mix of stereoisomers (often around half one type, and half another type), unlike our body, which only uses and makes one version.
Ketosis happens when blood ketones are higher than normal either through dietary changes (which lead to very low blood glucose) or through supplementation (independent of blood glucose concentrations).
Some people like to think of ketone bodies as the fourth energy source for humans (in addition to carbohydrates, fats and proteins).
That’s technically true, but the alcohol in booze (aka ethanol) can also be used for energy. Just because we can metabolize something doesn’t always mean we should.
Ketosis, which just means having more ketone bodies than normal, should not be confused with ketoacidosis, which is a potentially dangerous metabolic situation of uncontrolled ketosis.
Normally, our body is very good at self-regulating.
If it senses acid levels rising (as happens in ketosis), it responds by buffering with more alkaline molecules (such as bicarbonate), changing blood levels of CO2, absorbing hydrogen ions, or telling the kidneys to excrete more dihydrogen phosphate and ammonium ions.
However, if for some reason our body can’t compensate, and blood pH drops below about 7.35 (in other words, becoming more acidic), we’re in trouble.
This usually happens in diabetics and alcoholics, since their normal metabolic mechanisms may not work properly.
For the average healthy person, dietary ketosis or even brief fasting is generally safe.
How do we get into ketosis?
Method 1: Ketogenesis
We can make our own ketone bodies naturally, through the process of ketogenesis.
Our ancestors kicked off ketogenesis the good old fashioned way: by starving. About 72 hours into starvation, ketogenesis is happening and you’re in ketosis. Congratulations!
Ketosis is essentially an effect of fasting. This means that many of the health effects of fasting may be due to ketosis itself, rather than something like energy restriction.
Interestingly, how quickly ketosis happens varies by age and species.
Other mammals don’t seem to go into ketosis nearly as quickly as humans (your friendly neighborhood hibernating bear or squirrel who doesn’t eat for weeks to months at a time? No ketosis.)
Babies, on the other hand, go into ketosis within a few hours of not eating.
This may have to do with our energy-hungry human brains. About 20 percent of our overall energy intake is devoted to feeding our brains. Although bears and squirrels are clever enough to get into the garbage, they don’t have brains as large as we do.
It seems that ketogenesis is a human backup system that provides enough energy (via ketone bodies) to the ol’ noggin in times of starvation.
And it may be this particular evolutionary adaptation—which perhaps began as a way to keep the thinking factory upstairs working when food was scarce—that also enables the brain-benefiting effects of the ketogenic diet.
Stored glucose (our sugar-based fuel) is actually rather heavy. We don’t carry around much of it. Our body prefers to store most of our excess energy as body fat.
When we eat normally, our brain gets enough energy from glucose that can easily pass the blood-brain barrier.
When we stop eating, we run out of stored glucose (as glycogen) within 2-3 days (faster if we’re active), and have to find some other fuel source.
By the way, the relative heaviness of stored glycogen is why many people report fast weight loss on a ketogenic or low-carb diet: their body has dumped a little extra weight in the form of glycogen and water (which tags along with glycogen in a 3 parts water to 1 part glycogen ratio). Unfortunately, this water and glycogen comes right back once we start eating normally again.
Method 2: A ketogenic diet
Most people frown on starving children with epilepsy, so a ketogenic diet is the next best thing.
By cutting off the body’s carbohydrate (aka glucose) supply, but providing energy and nutrients in the form of fat (plus a little protein), we can get the same effects as straight-up starvation: ketosis.
As with starvation, it usually takes some time to get into ketosis once we stop eating carbs.
Many people like to measure their ketosis with Ketostix, which test for ketones in the urine. This is not always a reliable indicator, since all it tells you is whether you’re excreting excess ketones, not whether you’re actually in ketosis per se.
In addition, Ketostix only measure the presence of excreted acetoacetate, not the presence of D-β-hydroxybutyrate.
Over time, our body’s excretion of ketones can change, even if we’re still in ketosis. Therefore, you may see different readings on the Ketostix, regardless of what is actually happening in your body.
Method 3: Supplement with ketones
If ketones are what we want, why not just take them instead of making our own by fasting or cutting out carbohydrates?
Great idea, and totally new… except it isn’t.
As early as 1953, there were studies looking into whether we could “artificially” produce ketosis by supplementation.
Today, we know that by supplementing with ketone bodies (usually D-β-hydroxybutyrate or certain esters) you can raise the level of ketone bodies in the blood without being in ketogenesis.
This has a lot of cool possibilities. If ketone supplementation can give us the health benefits of ketosis without us having to fast / starve or follow a very restrictive diet, that could be a win-win.
Unfortunately, we still don’t have conclusive human studies on this that would give us clear direction. Check back in 10 years.
The buzz is that ketone supplements can make you thin and cure whatever ails you. But what you read about in the media or on the interwebs isn’t always what scientists actually found in the lab.
If you didn’t know better, you’d think ketone supplementation just started. Actually, research on this topic goes back to the 1950s. All of it has been conducted using rats. Here are the findings.
Weight loss
D-β-hydroxybutyrate supplementation made some types of rats eat less and lose weight, but not other types of rats.
Some evidence kinda sorta indicates that D-β-hydroxybutyrate supplementation might activate brown fat (a metabolically active fat that is, in part, responsible for thermogenic adaptations) via the sympathetic nervous system, but there was no follow-up.
Blood glucose regulation
Another showed that ketone supplementation with either 1, 3-butanediol acetoacetate diester or sodium/potassium β-hydroxybutyrate decreased blood glucose with no changes in cholesterol or blood triglycerides (the not-so-great side effects of the ketogenic diet).
Traumatic brain injury
In one study, infusing D-β-hydroxybutryate into adult rats after traumatic brain injuries showed improved energy (ATP) levels.
In another study, D-β-hydroxybutryate didn’t improve things and actually caused damage to the blood-brain barrier, even in healthy rats.
Epilepsy
New evidence suggests that it may not be D-β-hydroxybutryate or acetoacetate preventing seizures; rather, it might be the relatively short-chain fatty acids (nanoeic and decanoic acids) in the diets when on a ketogenic diet crossing the blood-brain barrier, inhibiting seizures.
But in another study that exposed rats to high-pressure oxygen containing ketone esters such as R,S-1,3-butanediol acetoacetate diester, the rodents saw increased blood β-hydroxybutryate and decreased seizures.
Cancer
A recent study found that ketone supplementation extended survival in mice with metastatic cancer. But while it’s true that most cancers have a highly anaerobic metabolism, this in not universal. If proven to be effective, it’s likely that ketone supplementation would be an additional treatment rather than a stand alone treatment for cancer, because of its robust nature.
For now, almost no studies on ketone supplementation have used human clinical trials. So if anyone tells you that ketone supplementation is a miracle cure, ask if you can get some for your pet rat… if it’s the right kind of rat.
Will ketosis help me?
Ketogenesis and ketosis are easy to study.
All you have to do is starve people, or feed them a high-fat/low-carb diet, and wait. Then you see if it changes whatever you’re interested in fixing.
Since we’ve known about fasting and ketosis for quite a long time, and it’s relatively easy to research, there are probably good reasons why it’s not yet considered a miracle cure.
And it’s not because Big Pharma or Carbohydrate Corporation or The Cancer Conspiracy have vested interests. (Trust me, we scientists can barely keep the grad students from contaminating the super-purified water by leaving the lid off the jug, never mind organize an evil cabal of ketosis deniers.)
To be fair, the introduction of anti-epileptic drugs in the late 1930s onward did lead to less interest in dietary ketosis as a treatment for epileptic children.
But we don’t yet use ketosis (or ketone supplementation) to fix everything from muffin tops to hangnails because:
- For many populations, ketosis has little or no effect.
- It may only work for particular types of people, with particular needs and health conditions.
- It may take too long to see a measurable effect.
- For many people, a ketogenic diet is too hard to consistently follow.
That being said, here are some interesting and promising new avenues for ketosis… as well as some “don’t bother” examples.
Probable benefit: Metabolic diseases
We know that fasting is often an effective short-term treatment for metabolic dysfunction such as poor glucose control / early Type 2 diabetes, chronic inflammation, or hypertension.
We don’t know for sure yet whether this is because of ketosis or some other mechanism (such as programmed cell death, aka apoptosis).
However, research suggests that in some cases, such as type 2 diabetes, ketosis may be useful as a short-term treatment or a “boost” that helps return metabolic processes back to a more normal and well-regulated state.
In these specific situations, a ketogenic diet or a structured intermittent fasting program done under close medical supervision for a specific objective, may be a useful as part of a multi-pronged treatment program that probably should include other therapeutic tools such as medication or other well-established health procedures.
Notice all our italics here. What we mean is:
- Don’t use ketosis or fasting alone to try to cure stuff.
- Don’t use ketosis or fasting just to randomly “get healthy”.
- “Medical supervision” does not mean Dr. Google.
Verdict: Could help in some cases, but should be done with a clear purpose and carefully monitored. Not a long-term “cure-all” for most people.
Why does ketosis seem to help some types of metabolic dysfunction?
Ketones may help, in part, because they decrease oxidative stress, boost antioxidants and scavenge free radicals.
Oxidation is a natural part of cellular metabolism, but too much oxidation, too fast, without the balance of antioxidants, contributes to many metabolic and other diseases.
Many metabolic disorders are related to this process of oxidation, in which our cells essentially “rust” from the inside. If we can slow and regulate oxidation, it may improve our health and longevity.
Probable benefit: Neurodegeneration and brain injuries
We know ketosis for epilepsy is a win—can ketosis help other types of brain illnesses and injuries?
Recent research suggests that many brain disorders (such as Alzheimer’s and Parkinson’s, among other neurodegenerative diseases) are related to other metabolic disorders such as diabetes, obesity, non-alcoholic fatty liver disease (NAFLD).
These metabolic and neourodegenerative diseases show common features, such as oxidative stress, mitochondrial dysfunction, and inflammation. In fact, Alzheimer’s is now often described as “diabetes of the brain”, or “Type 3 diabetes”.
The presence of ketones also seems to improve outcomes from traumatic brain injury (TBI). However, right now, most of these studies have been done on rats.
Still, based on what we’ve seen with epilepsy and rat studies, chances are good that ketones may be a low-risk treatment—and perhaps even a preventive strategy—to improve brain health. See above about getting medical supervision from someone other than Dr. Google.
Verdict: Probably can’t hurt, might help people with neurodegeneration and/or mild to moderate brain injury.
Unclear benefit: Longevity
We know that caloric restriction (CR) improves longevity in most organisms studied. We know that intermittent fasting seems to have some of the same benefits, sometimes.
But right now, we don’t know if ketosis works the same way.
The real question here is: Who’s willing to find out?
Would you stick to a ketogenic diet in the name of advancing knowledge, achieving scientific glory as a “ketonaut”? Most of us wouldn’t.
Plus, without a control group (say, your identical twin who lives exactly the same lifestyle as you, in the exact same environment, with only your diets being different), it’s hard to know for sure whether your 100th birthday was due to ketosis or something else.
For now, any longevity benefits would be mostly speculative. And your 100th birthday cake would have to be a block of butter.
Verdict: You could try this one and get your next of kin to report back… but most people wouldn’t want to.
Interesting, but probably no advantage for most people: Athletic performance
Athletes need fuel to perform.
Could we possibly enable people to tap into their stored body fat more effectively, and require less re-fueling from stuff like sugary energy gels?
Ketosis lets you avoid glycogen depletion (aka bonking, hitting the wall), because you aren’t using glycogen as your energy source, so you don’t need to take in carbs as you compete. Instead you’re using fat and ketone bodies. You increase fat oxidation, spare glycogen, produce less lactate and use less oxygen at submaximal rates.
All this sounds great, but the exercise physiologists’ consensus is that while all these adaptations are true, the problem is that with fat and ketone bodies as fuel, you’re not going to go as fast as you can when using with glucose and carbohydrates.
The bottom line for athletes is performance, and so far there is only one very new study showing a small improvement in cyclist’s performance with ketone supplementation combined with carbohydrate supplementation (compared to just carbohydrate supplementation alone).
It seems that combining ketones with carbs, rather than exclusively using one or the other, might offer some benefit.
A recent study compared the effect of drinking just carbs to drinking carbs + ketones in male and female elite cyclists.
After not eating overnight (about 16 hours) the cyclists came to the lab and drank either a carb drink or a carb + ketone (c + k) drink.
Carb drink:
- 40% dextrose
- 40% fructose
- 20% maltodextrin
C + k drink
- 60% dextrose
- 40% ketone ((R)-hydroxybutyl (R) -3-hydroxybutyrate ketone ester).
Total amount of substrate in both drinks were 573 mg/kg body weight.
The cyclists drank half of their drink, rode for 1 hour at 75% of their max power output. Then they drank the other half of their drink and biked as far as they could in 30 minutes.
After a week, the cyclist repeated the experiment with the opposite drink.
Results
When drinking the c + k drink the cyclists biked, on average, 2 percent (400 meters) farther longer over the 30 minutes.
There were some metabolic differences to note in with the c+k drink:
- less lactate
- more fatty acids in the blood
- more D- β- hydroxybutyrate
Bottom line: Supplementing with a combination of carbohydrates and ketones may improve performance in aerobic competitions.
Verdict: Some intriguing possibilities, particularly for aerobic performance, but to date there very little evidence to improve overall athletic performance.
No real advantage: Losing fat
Oh, insulin, you naughty monkey! You have been getting yourself in so much trouble lately!
Low-carb advocates in the late 1990s and early 2000s thought maybe they had stumbled on the key to fighting flab: insulin. Insulin is mainly a storage hormone: Its job is basically to help nutrients get into cells.
The low-carb / insulin hypothesis, dramatically oversimplified, went like this:
- Insulin makes stuff go into cells.
- Stuff that goes into fat cells makes us fat.
- If we don’t help stuff go into cells, then we won’t get fat. We might even lose fat.
- Carbs (in their digested form of glucose) stimulate insulin release.
- Therefore eating fewer carbs = less body fat.
Now, this theory did have some merits.
For one thing, it got some of us unhooked from processed sugary and starchy treats, and thinking more about fiber content and healthy fats.
Unfortunately, insulin is not the only player. There’s never only one player in the team sport and complex system that is your body.
Nor does insulin act alone. Energy storage is governed largely by our brain, not a single hormone.
The other upside to the low-carb approach was that people often ate more protein and more fat. When we eat protein and fat, we release satiety hormones, particularly CCK, which is one of the main hormones that tells us we’re full.
More protein and fat means we’re often less hungry. Which means we eat less. Which means we lose fat. It’s the “eating less” part (not the insulin part) that actually matters.
On top of this, if you’ll recall, carbohydrates are relatively heavy to store. Lower the carb intake, and our body will eventually release some water and glycogen.
Result: Weight loss. Magic!
Yet being in ketosis doesn’t seem to have any special advantage for losing body fat (rather than just weight), especially if we consider the lifestyle and behavior aspect to this.
You may find it easy to eat less when all you can eat is protein and fat. But after a while, you may grow tired of bringing your own whole salmon to parties, and wonder what the other 95% of the grocery store is up to. You may start to have fantasies about a threesome: you, Oreos, and chocolate sauce. Not only that, you may be getting some serious scurvy and other nutrient deficiencies.
For women in particular, lowering carbohydrate intake seems to have negative effects.
Women’s bodies go on high alert faster when they sense less energy and fewer nutrients coming in. Many women have found that the low-carb diet that worked great for their husband not only didn’t work for them, but it knocked out their menstrual cycle on the way out the door.
Verdict: We don’t recommend the ketogenic diet for sustainable fat loss.
As part of the carb-insulin hypothesis, people thought that maybe metabolism would also increase during ketosis.
A recent study looked at whether or not there was a significant increase in metabolic rate when going from a high-carbohydrate diet (48% carbohydrate) to a ketogenic diet (6% carbohydrate), with protein being the same (around 16-17%).
With this dietary change, insulin went down while fatty acids and ketone bodies went up. Basal metabolism (energy expenditure) went up by about 100 kcal per day.
Seems obviously good—but not so fast.
Figuring out what this actually means is complicated.
Researchers had to correct metabolism based on body weight, which as you’ve read, tends to drop when water is lost on low-carb diets.
The authors concluded that while there was a small increase in metabolism initially, that disappeared over the four weeks while insulin levels were still low.
So their study didn’t support the insulin-carb hypothesis.
Is protein actually the key factor?
The authors of the study think that differences found in other studies comparing high and low-carb diets are because of differences in protein intake rather than carbohydrate intake in those studies.
Protein promotes satiety and takes the most energy to digest and absorb, so differences in weight loss may be net calories absorbed, rather than decreases in insulin or increases in metabolism.
Definitely no advantage: Gaining lean mass
As you may have read above, insulin is mainly a storage hormone. It’s also considered an anabolic hormone. As in building things. As in getting swole.
For the most part, we need insulin—along with other hormones, such as growth hormone and testosterone—to create an anabolic, muscle-building environment. Trying to build muscle while in ketosis is like stepping on the gas and the brake at the same time.
However, as with athletic performance, we may discover that there is some benefit to supplementary ketones while building muscle. We don’t know yet.
Verdict: Build muscle with a more appropriately anabolic diet that includes carbohydrates (particularly around training), and supplement with ketones if you want to experiment.
What this means for you
If you’re a “regular person” who just wants to be healthy and fit:
- Enjoy reading about ketosis if you like. Try it, if you’re curious. But you can be perfectly fit, lean, and healthy without it.
- Don’t believe everything you read on the internet. (Except this article, of course.) Remember that the plural of “personal anecdote” is not “scientific data”. Be a critical reader and consumer.
If you’re an athlete:
- Know your body and the demands of your sport. Unless you’re an ultra-endurance athlete, becoming fat-adapted or adopting a ketogenic diet probably won’t improve your performance.
- Don’t add stress. Training is a good stress, but still a stressor. Fasting and restricting energy (i.e. calories) or a particular nutrient are also stressors. Stress adds up. Don’t add nutritional stress from a stringent diet to the mix, particularly if you’re female.
- Make meeting your nutritional needs your priority. If you’re active, you need more fuel and nutrients than the average person. Rather than taking stuff out of your diet, look for where you can add good stuff in: protein, vitamins, minerals, fiber, fatty acids, phytonutrients, water, etc. from whole, minimally processed foods.
If you’re a fitness professional / nutrition coach:
- Understand the basics of ketosis, ketogenic diets, and ketone supplementation. Know when, how, and for whom ketosis might be appropriate. If in doubt, learn more from trusted medical and research sources—which, again, does not include random people of the Internets.
- Help people understand as much as they need to understand in order to make an informed choice, with your guidance. Your clients will likely have questions. Prepare your answers in advance.
- Refer out: If you think a client might benefit from a ketogenic diet or ketone supplementation for a health condition, work with their doctor to support things like meal planning and keeping a food journal that looks for correlations between diet and how they feel.
- Stay within your scope of practice. Remember: Unless you’re licensed for medical nutrition therapy, you’re not authorized to prescribe any type of diet for medical conditions. Don’t tell your client that they should go on a keto diet to cure their diabetes.
If you have a specific health problem that a ketogenic diet (or ketone supplementation) may help with:
- Consult your doctor first. Discuss any research findings or potential dietary modifications with someone who actually went to med school. If you’re on any medications, make sure nothing you do will interfere with their effect.
- Carefully monitor and track any dietary modifications. First, you want to stay safe; second, you want to know if what you’re doing is having any effect. So decide how you’ll know if your dietary changes are “working”, and track those indicators closely.
- Consider coaching. Again, nutrition coaches are generally not qualified to offer medical nutrition therapy. However, they do know how to make fat and protein taste delicious, and how to help you organize your shopping and meal planning habits. For this and any other dietary modification, it helps to get some guidance.
SOURCE:
By Krista Scott-Dixon, Ph.D. and Helen Kollias, Ph.D.
"The ketogenic diet: Does it live up to the hype,"
https://www.precisionnutrition.com/ketogenic-diet
References:
Arnott, Robert, Stanley Finger, and Chris Smith. Trepanation: History, Discovery, Theory. The Netherlands: Swets and Zeitlinger, 2003.
Asadi-Pooya AA, Nikseresht AR, Yaghoubi E. Old Remedies for Epilepsy: Avicenna’s Medicine. Iranian Red Crescent Medical Journal. 2012;14(3):174-177.
Bailey EE, Pfeifer HH, Thiele EA. The use of diet in the treatment of epilepsy. Epilepsy Behav. 2005 Feb;6(1):4-8.
Chang P, Augustin K, Boddum K, Williams S, Sun M, Terschak JA, Hardege JD, Chen PE, Walker MC, Williams RS. Seizure control by decanoic acid through direct AMPA receptor inhibition. Brain. 2016 Feb;139(Pt 2):431-43.
Cox PJ, Kirk T, Ashmore T, Willerton K, Evans R, Smith A, Murray AJ, Stubbs B, West J, McLure SW, King MT, Dodd MS, Holloway C, Neubauer S, Drawer S, Veech RL, Griffin JL, Clarke K. Nutritional Ketosis Alters Fuel Preference and Thereby Endurance Performance in Athletes. Cell Metab. 2016 Jul 26. pii: S1550-4131(16)30355-2. doi: 10.1016/j.cmet.2016.07.010. [Epub ahead of print]
Cox PJ, Clarke K. Acute nutritional ketosis: implications for exercise performance and metabolism. Extreme physiology & medicine. 2014 Oct 29;3(1):1.
D’Agostino DP, Pilla R, Held HE, Landon CS, Puchowicz M, Brunengraber H, Ari
C, Arnold P, Dean JB. Therapeutic ketosis with ketone ester delays central
nervous system oxygen toxicity seizures in rats. Am J Physiol Regul Integr Comp
Physiol. 2013 May 15;304(10):R829-36.
Greco T, Glenn TC, Hovda DA, Prins ML. Ketogenic diet decreases oxidative stress and improves mitochondrial respiratory complex activity. Journal of Cerebral Blood Flow & Metabolism. 2015 Oct 13:0271678X15610584.
Hall KD, Chen KY, Guo J, Lam YY, Leibel RL, Mayer LE, Reitman ML, Rosenbaum M, Smith SR, Walsh BT, Ravussin E. Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Am J Clin Nutr. 2016.
Hashim SA, VanItallie TB. Ketone body therapy: from the ketogenic diet to the oral administration of ketone ester. J Lipid Res. 2014 Sep;55(9):1818-26. doi: 10.1194/jlr.R046599.
Henderson ST. Ketone bodies as a therapeutic for Alzheimer’s disease. Neurotherapeutics. 2008 Jul;5(3):470-80. doi: 10.1016/j.nurt.2008.05.004.
Hertz L, Chen Y, Waagepetersen HS. Effects of ketone bodies in Alzheimer’s disease in relation to neural hypometabolism, β-amyloid toxicity, and astrocyte function. J Neurochem. 2015 Jul;134(1):7-20. doi: 10.1111/jnc.13107.
Hippocrates, Epidemics VII, 46.
Jha SK, Jha NK, Kumar D, Ambasta RK, Kumar P. Linking mitochondrial dysfunction, metabolic syndrome and stress signaling in neurodegeneration. Biochim Biophys Acta. 2016 Jun 21. pii: S0925-4439(16)30157-0. doi: 10.1016/j.bbadis.2016.06.015.
Kesl SL, Poff AM, Ward NP, Fiorelli TN, Ari C, Van Putten AJ, Sherwood JW,
Arnold P, D’Agostino DP. Effects of exogenous ketone supplementation on blood
ketone, glucose, triglyceride, and lipoprotein levels in Sprague-Dawley rats.
Nutr Metab (Lond). 2016 Feb 4;13:9
Kolanowski J, Young JB, Landsberg L. Stimulatory influence of D(-)3-hydroxybutyrate feeding on sympathetic nervous system activity in the rat. Metabolism. 1994 Feb;43(2):180-5.
Orhan N, Ugur Yilmaz C, Ekizoglu O, Ahishali B, Kucuk M, Arican N, Elmas I,
Gürses C, Kaya M. Effects of beta-hydroxybutyrate on brain vascular permeability
in rats with traumatic brain injury. Brain Res. 2016 Jan 15;1631:113-26.
Pinckaers PJ, Churchward-Venne TA, Bailey D, van Loon LJ. Ketone Bodies and Exercise Performance: The Next Magic Bullet or Merely Hype? Sports Med. 2016 Jul 18. [Epub ahead of print]
Poff AM, Ari C, Arnold P, Seyfried TN, D’Agostino DP. Ketone supplementation
decreases tumor cell viability and prolongs survival of mice with metastatic
cancer. Int J Cancer. 2014 Oct 1;135(7):1711-20.
Pugazhenthi S, Qin L, Reddy PH. Common neurodegenerative pathways in obesity, diabetes, and Alzheimer’s disease. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease. 2016 May 6.
Volek JS, Noakes T, Phinney SD. Rethinking fat as a fuel for endurance exercise. Eur J Sport Sci. 2015;15(1):13-20. doi: 10.1080/17461391.2014.959564.
Wheless, J. W. (2008), History of the ketogenic diet. Epilepsia, 49: 3–5. doi:10.1111/j.1528-1167.2008.01821.x
Wilder RM. (1921) The effect on ketonemia on the course of epilepsy.Mayo Clin Bull 2:307.
Woodyatt RT. (1921) Objects and method of diet adjustment in diabetics. Arch Intern Med28:125–141.
You Might Also Enjoy...


How NightLase® Can Help With Snoring

How Laser Therapy Can Help Decrease Vaginal Dryness and Increase Sexual Pleasure

Five Signs You Could Be Suffering From Low Testosterone

Why Do I Still Get Acne, and How Can I Get Rid of It Without Medication?


